Different rodent species (e.g. mice and rats), shrews, moles and bats are the natural hosts of hantaviruses. Infected rodents excrete the virus with saliva, urine and feces.
Transmission of rodent-borne hantaviruses to humans (zoonoses) usually occurs indirectly by inhaling virus-contaminated dust – direct contact with rodents is not necessary. Outside the host, the viruses remain infectious for up to approximately two weeks. In humans, hantavirus infection can cause severe disease causing nephrological damage and even kidney failure.
In Germany, most human hantavirus disease cases are caused by the Puumalavirus which is transmitted by bank voles. In the Eastern part of Germany, where the striped field mouse is endemic, also human infections with Dobrava-Belgrade virus have been reported.
The current number of reported hantavirus disease cases can be found on the website of the Robert Koch-Institute under SurvStat.
Further information on human hantavirus infections can be found in the RKI information sheet (in German language, for download in the right column of this webpage).
Veterinary issues of this infectious disease are handled by the National Reference Laboratory for hantaviruses at the Friedrich-Loeffler-Institut.
Aktuelle Untersuchungsergebnisse des RoBoPub-Zoonoseforschungsverbundes („Rodent-Borne-Pathogens-and-Public-Health“, d.h. Nagetier-übertragene Krankheitserreger und öffentliche Gesundheit) deuten darauf hin, dass im laufenden Jahr im Landkreis Osnabrück mit einer erhöhten Zahl humaner Erkrankungen gerechnet werden muss. Darauf weisen eine erhöhte Rötelmauspopulation und eine hohe Verbreitung des Puumala-Orthohantavirus (PUUV) in den Rötelmäusen hin. Die Zahl der bisher gemeldeten Erkrankungsfälle im Landkreis Osnabrück übertrifft bereits die Gesamtzahl aller gemeldeten Fälle vom Vorjahr (Stand: 21. Kalenderwoche). Dies geht insbesondere aus den vom Niedersächsischen Landesamt für Verbraucherschutz und Lebensmittelsicherheit (LAVES), dem Gesundheitsamt Osnabrück, dem Niedersächsischen Landesgesundheitsamt (NLGA), dem Julius Kühn-Institut (JKI), dem Institut für Medizinische Virologie der Charité und dem Friedrich-Loeffler-Institut (FLI) gesammelten Daten hervor. Gegenwärtig konzentrieren sich die RoBoPub-Partner JKI und FLI auf die Untersuchung der Situation in weiteren Endemiegebieten, um eine Prognose auch für diese Regionen geben zu können.
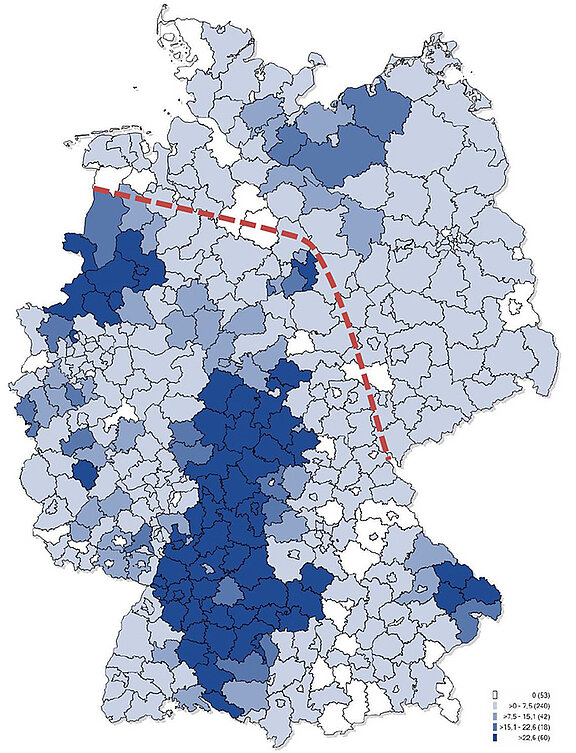
Hantaviren verursachen beim Menschen eine fiebrige, grippeähnliche Erkrankung, die bei schweren Verläufen mit Nierenfunktionsstörungen verbunden sein kann. In Deutschland unterliegt der Nachweis von Hantaviren seit Einführung des Infektionsschutzgesetzes im Jahr 2001 der Meldepflicht, soweit er auf eine akute Infektion hinweist. Auch das klinische Bild eines akuten viralen hämorrhagischen Fiebers ist meldepflichtig. Die Zahl der jährlich gemeldeten Hantavirusfälle zeigt starke Schwankungen mit deutlich erhöhten Zahlen in den „Ausbruchs“-Jahren 2007, 2010, 2012 und 2017. Die humanen Hantaviruserkrankungen in Deutschland werden vor allem durch das Puumala-Orthohantavirus (PUUV) verursacht. Der Reservoirwirt dieses Hantavirus ist die Rötelmaus. Endemiegebiete, das heißt Regionen, in denen häufig über lange Zeiträume Infektionen mit dem PUUV auftreten, liegen im westlichen und südlichen Teil Deutschlands, insbesondere in bestimmten Gebieten von Baden-Württemberg, Bayern, Niedersachsen, Nordrhein-Westfalen und Hessen (Karte). Auf diese Regionen beschränkt sich auch die Verbreitung des PUUV; im östlichen Teil Deutschlands kommt dieses Hantavirus nicht vor. Die gegenwärtig bekannte Verbreitungsgrenze verläuft in Niedersachsen, Hessen/Sachsen-Anhalt und Thüringen (Karte).
In den genannten Endemiegebieten infizieren sich Menschen verstärkt während Massenvermehrungen der Rötelmaus, die i.d.R. im Jahr nach einer Buchenmast (massenhafte Produktion von Bucheckern) auftreten.
Leider ist gegen die Hantavirusinfektion kein Impfstoff verfügbar. Deshalb kommt der Expositionsprophylaxe große Bedeutung zu. Hinweise dazu sind im Merkblatt „Wie vermeide ich Hantavirusinfektionen?“ dargestellt.
Joint information of the JKI, RKI, FLI and National Consiliary Laboratory for Hantaviruses at the Charité on the respective homepages
04 March 2012
Scientists and forestry agencies have registered signs of a possible increase in hantavirus infections in 2012. As a rule, this infectious disease which is mainly transmitted by bank voles has a mild course with flu-like symptoms; in isolated cases however severe courses of disease with kidney failure requiring dialysis may occur. According to the forestry agencies, beeches and oaks particularly in Baden-Wuerttemberg, Hesse, Bavaria, Northrhine-Westphalia, Lower Saxony and Thuringia produced a particularly large number of fruit („full mast“) last year, which might lead to an increase in the number of bank voles. In the frame of a study in Baden-Wuerttemberg carried out in autumn 2011, the Friedrich-Loeffler-Institut and the Julius Kühn-Institut detected a high population density of bank voles which might lead to an explosion of the population this year. Over the past few months, the Robert Koch-Institut also has registered an increase in human hantavirus infections which are notifiable to the local health authorities pursuant to the Infection Protection Act. In most years, the number of infections decreases after a peak in summer; during the past autumn and winter season however this was not the case. A similar phenomenon was observed at the turn of the year 2009/2010 prior to the hantavirus outbreak year 2010. Again, regions with known hantavirus endemic areas (e.g. the Swabian Alb, the Bavarian Forest, the area around Osnabrück, the Münsterland) are particularly affected.
In Germany, hantavirus infections have been known since the mid-1980s. Since mandatory notification was introduced in 2001, an annual average of 500 cases has been reported. Data collected Europe-wide reveal that a significant increase in the number of infections must be expected at regular intervals of 2 to 3 years. Such increases were observed in Germany in 2007 and 2010 with 1688 and 2017 cases, respectively. These outbreaks were mainly caused by a hantavirus called Puumalavirus which is transmitted to humans by bank voles. The reasons for the strong fluctuations in the number of notified cases are unclear. An association with the population density of bank voles and their hantavirus infection rate is likely. A strong fruit production (mast) of beeches and other relevant tree species plays a crucial role for the population dynamics of rodents. An increased availability of food caused by the beech mast increases the survival probability of bank voles in the winter half-year. In extreme cases, rodents even might reproduce in winter, which might lead to an increase in the population density at the beginning of the subsequent year. These populations will then begin to reproduce further in spring and may be the source of human infections, if their infection rate is sufficiently high.
Hantavirus disease in humans begins with increasing fever, headaches as well as back and abdominal pain. Often, vision disorders occur. In severe cases, a drop in blood pressure and dysfunction of internal organs, especially kidney failure, are observed over the next days. Blood tests show a reduction of the thrombocyte count and an increase in serum creatinine; in urine samples protein and red blood cells are detected frequently. As a rule, the patient will recover completely, once the clinically critical phase has been overcome.
Detection of hantavirus antibodies in the blood is used for specific diagnostics. Analysis of the genetic material of the virus, which is only detectable in the patient’s blood during the first 1 to 3 weeks of disease, is of particular importance. Physicians and diagnostic laboratories are kindly asked to contact the national consiliary laboratory for hantaviruses at the Charité.
Further information and tips for prevention can be found in the information sheet „Informationen zur Vermeidung von Hantavirus-Infektionen“, which is available on the homepages of the Charité, FLI, JKI and RKI.
04. August 2010: This year a total of 1,318 laboratory confirmed cases of hantavirus disease were registered until August 4, the majority of them in Baden Württemberg (739) and Bavaria (249), followed by Northrhine-Westphalia (98), Hesse (94), and Lower Saxony (76) (Robert Koch-Institut: SurvStat, http://www3.rki.de/SurvStat, as per August 4, 2010). So far, the highest number in Germany occurred in 2007; in the subsequent years 2008 and 2009 the numbers were considerably lower with 243 and 181 cases, respectively (Fig. 1).
Currently, no reliable statement can be made on the reasons for the considerable increase in notified cases this year (and in 2007). One factor may be the strong increase in the number of bank voles due to a beech mast last year. For elucidation, a cooperation project has been started to conduct long-term studies on the population dynamics of bank voles, the presence of Puumalavirus (one of the three hantavirus types in rodents in Germany) in the bank vole population and the incidence of human infections. One of the aims of these investigations is to develop a long-term monitoring program for early detection of signs of an increased infection risk for the human population. Project partners are the Julius Kühn-Institute, the Friedrich-Loeffler-Institut, the Robert Koch-Institute, the National Consiliary Laboratory for Hantaviruses at the Institute of Virology of the Charité, the State Health Agency Baden-Württemberg, the Bundeswehr Institute for Microbiology and the Büsgen-Institut of the University of Göttingen.

In the North and East of the country, the Dobrava-Belgrade-Virus transmitted by the striped field mouse (Figure 2B) also causes human infections.
Typically, the clinical course of a hantavirus infection is characterized by high fever, headaches, backaches and abdominal pain, drop in blood pressure and kidney disorders. In some cases, extrarenal manifestations of a hantavirus infection can be observed, mainly accompanying hepatitis or involvement of the lung. Many cases of disease, however are not recognized as such, either because an infectious cause for kidney failure is not considered or the technical preconditions for virus diagnostics are not available.
Persons who live in the known endemic areas and who have contact with rodents and their excretions due to their profession or their living conditions have an increased risk of infection. Risk factors for transmission of hantaviruses from the reservoir animal to humans are outdoor activities (forest, field, construction sites), forest and park areas in the immediate vicinity of living quarters as well as increased contact to mice and their excretions. As so far no protective vaccination and no causative antiviral therapy are available, exposure prophylaxis is of utmost importance.
The best protection from infections is to avoid contact with the excretions of rodents. This includes keeping mice away from living quarters and their closer environment (e.g. by avoiding the accumulation of food waste close to residential buildings). Also farmers and stud workers should thoroughly prevent mice from settling and eliminate mouse nests in the animal houses (please use gloves and masks, avoid to disperse mouse excretions, disinfection).
An infection risk also arises from re-opening and cleaning summer houses after the winter; these should be aired out thoroughly prior to cleaning (if necessary by applying the same safety measures as in animal houses).
For further information please refer to the information sheet „Wie vermeide ich Hantavirusinfektionen“ (How to avoid hantavirus infections) and to the links below:
- www.rki.de > Infektionskrankheiten A-Z > Hantavirus-Infektionen
- http://www.charite.de/virologie/
- http://www3.rki.de/SurvStat/
Authors:
- Detlev H. Krüger (IMV, Charité Berlin)
- Rainer G. Ulrich (FLI, Greifswald-Insel Riems)
- Jens Jacob (JKI, Münster)